Menopause is a deeply individual journey, shaped by biology, lifestyle, and personal values. No two women experience it the same way. Some navigate the transition with minimal disruption, while others face an onslaught of physiological and psychological turbulence—ranging from insomnia to joint pain, memory lapses to mood swings. This unpredictable nature has propelled a surge in demand for personalized wellness plans blending conventional and alternative approaches.
The days of one-size-fits-all menopause care are fading. What’s emerging in their place is a more nuanced, patient-centered model—one that respects the complexity of hormonal decline and empowers women to tailor treatment strategies to their unique needs.
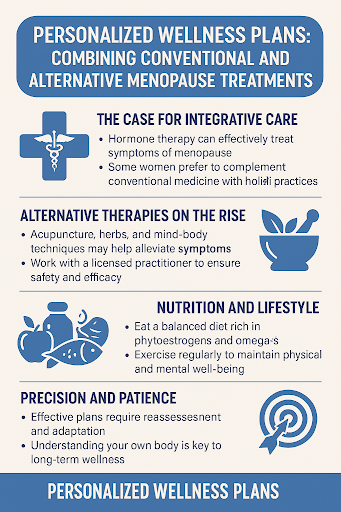
The Case for Integrative Care
Standard medical protocols have long centered on hormonal solutions, for good reason. The benefits of estrogen replacement are well-documented in the scientific literature. This therapy alleviates vasomotor symptoms, enhances bone density, and helps regulate mood disturbances linked to hormonal fluctuations. When appropriately prescribed, estrogen therapy can dramatically improve quality of life and mitigate long-term health risks such as osteoporosis and cardiovascular disease.
Yet for some women, hormone therapy is not a viable option, due to personal choice, family history, or contraindications like breast cancer risk. Others seek to complement conventional medicine with more holistic or culturally aligned practices. Thus, integrative care becomes not just an alternative but a necessity.
Alternative Therapies on the Rise
From acupuncture to adaptogenic herbs, alternative therapies have seen a renaissance among midlife women. These treatments do not replace evidence-based interventions but exist in conversation with them. For example, black cohosh and red clover are frequently used to ease hot flashes. Ashwagandha has been explored for its role in stress modulation. Mind-body techniques such as meditation, breathwork, and tai chi can regulate cortisol and improve sleep quality.
Importantly, these therapies must be vetted with the same rigor as pharmaceuticals. Not all supplements are created equal, and quality control remains a significant concern. Collaborating with a licensed integrative health practitioner ensures safety and alignment with overall health goals.
The Role of Data and Diagnostics
Personalized menopause care begins with comprehensive diagnostics. Hormone panels, bone scans, metabolic assessments, and even genomic data can provide a roadmap for tailoring treatments. Baseline evaluations help pinpoint deficiencies and predict how a woman’s body may respond to interventions.
Functional medicine clinics often go further, analyzing gut health, micronutrient levels, and inflammatory markers. These data points are used to design multifaceted plans beyond symptom suppression, focusing instead on root-cause resolution and long-term vitality.
For women receiving the benefits of estrogen replacement, these assessments can also inform optimal dosage and delivery methods—be they patches, pills, or gels—and allow for adjustments based on real-time physiological feedback.
Nutrition and Lifestyle: The Foundational Pillars
At the core of every personalized wellness plan is lifestyle. Nutrition, in particular, plays a foundational role. Diets rich in phytoestrogens (found in flaxseeds, soy, and legumes), omega-3 fatty acids, and antioxidant-laden produce can naturally modulate estrogen activity and reduce inflammation.
Equally important is removing endocrine disruptors—chemicals found in plastics, cosmetics, and even household cleaners—that may interfere with hormonal balance.
Sleep hygiene, stress reduction, and consistent physical activity are not optional extras; they are essential interventions. A woman who optimizes these areas may see magnified results from conventional and alternative treatments.
Navigating the Emotional Terrain
Menopause often stirs deeper questions of identity, purpose, and emotional resilience. Psychotherapy, particularly cognitive behavioral therapy (CBT), has demonstrated efficacy in managing anxiety and depression during this life stage. Journaling, creative expression, and community support circles provide additional outlets for emotional processing.
The modern wellness plan acknowledges these psychosocial dimensions and includes emotional wellness as a central component—not a fringe concern.
Even for those experiencing the benefits of estrogen replacement, emotional support can amplify outcomes and foster a deeper sense of self-trust during a period marked by rapid transformation.
Precision and Patience
Personalized care is not fast-track. It is iterative by nature. What works one month may require recalibration the next. Hormone levels shift, life stressors change, and tolerance to certain treatments may evolve.
This is where health literacy becomes power. Understanding one’s body, recognizing subtle signs of imbalance, and having access to responsive care providers ultimately drive long-term success.
An effective wellness plan includes periodic reassessment, open communication between patient and provider, and a willingness to adapt.
A Future of Empowered Menopause Care
As societal taboos surrounding menopause begin to erode, a new era is emerging—one where women are not merely surviving the transition, but actively reclaiming it as a season of empowerment.
The benefits of estrogen replacement, when paired with complementary therapies and a lifestyle rooted in self-awareness, offer not just symptom relief, but an invitation to thrive. Personalized wellness plans are no longer a luxury for the few; they are an imperative for the many.
In an age where customization defines everything from streaming playlists to skincare routines, it only makes sense that menopause care should follow suit—crafted not for the average patient, but for the individual woman, in all her complexity.



